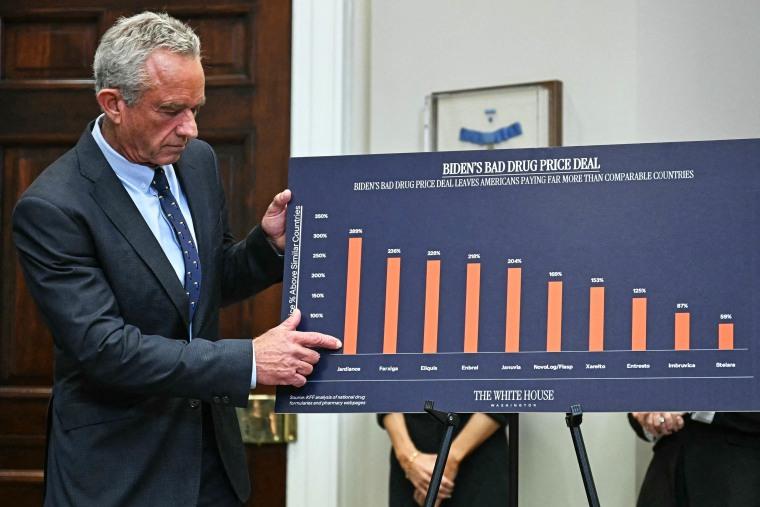
Analyzing the Impact of TrumpŌĆÖs Prescription Drug Pricing Plan Amidst Ongoing U.S. Healthcare Challenges
Regulatory Pressure Without Legislative Authority: The Core of TrumpŌĆÖs Drug Pricing Approach
Former President Donald TrumpŌĆÖs initiative to reduce prescription drug prices in the United States primarily depended on regulatory actions rather than comprehensive legislative reforms. This strategy focused on leveraging federal agencies to apply pressure on pharmaceutical companies, yet it lacked the robust congressional support necessary to enforce lasting changes. Without binding laws, these regulatory efforts often amounted to warnings rather than mandates, limiting their ability to disrupt entrenched pricing structures within the pharmaceutical sector.
Key limitations of this approach include:
- Dependence on executive orders and agency directives vulnerable to legal challenges
- Absence of bipartisan consensus essential for sustainable policy implementation
- Pharmaceutical firmsŌĆÖ capacity to navigate around regulations and contest enforcement actions
| Regulatory Strategy | Potential Effectiveness | Pharmaceutical Industry Reaction |
|---|---|---|
| Mandates for Pricing Transparency | Low to Moderate | Legal pushback and limited price adjustments |
| Importing Lower-Cost Medications | Moderate | Concerns over supply chain integrity |
| Enhanced FDA Oversight | Variable | Faster approval of generic drugs |
Enforcement Gaps Undermine the Effectiveness of Pricing Initiatives
Despite assertive rhetoric, TrumpŌĆÖs drug pricing plan largely relied on voluntary cooperation from pharmaceutical companies, which raised doubts about its capacity to drive meaningful cost reductions. The absence of enforceable penalties meant that the administrationŌĆÖs threats often remained symbolic, lacking the legal teeth to compel manufacturers to revise their pricing strategies significantly.
Furthermore, the planŌĆÖs emphasis on indirect tacticsŌĆösuch as promoting negotiation and transparencyŌĆöfell short without empowered regulatory bodies or clear statutory authority. This reliance on goodwill from stakeholders, who have historically resisted pricing reforms, further weakened the planŌĆÖs potential impact.
- No compulsory price limits: Drugmakers could disregard recommendations without facing consequences.
- Insufficient federal oversight: Regulatory agencies lacked the authority to enforce compliance effectively.
- Voluntary data disclosure: Transparency efforts depended on self-reporting by pharmaceutical companies.
| Enforcement Mechanism | Level of Enforcement | Likely Outcome |
|---|---|---|
| Encouragement of Price Negotiations | Low | Relies on voluntary participation |
| Transparency Programs | Medium | Enhances consumer awareness |
| Threatened Sanctions | Minimal | Uncertain enforcement follow-through |
Pharmaceutical IndustryŌĆÖs Pushback: Identifying Loopholes and Resistance Tactics
Industry representatives quickly criticized the administrationŌĆÖs drug pricing framework, pointing out its dependence on indirect measures rather than enforceable mandates. They contended that the planŌĆÖs regulatory threats lacked substantive authority, enabling drug manufacturers to maintain their pricing models with little disruption. Lobbyists highlighted several weaknesses in the proposal that could be exploited to sustain high medication costs.
Major industry concerns include:
- Narrow focus: The plan excluded many patented specialty drugs, limiting its overall reach.
- Voluntary adherence: Many initiatives depended on the pharmaceutical sectorŌĆÖs willingness to comply, reducing effectiveness.
- Prolonged appeals: ManufacturersŌĆÖ ability to challenge pricing decisions could delay any immediate cost relief.
| Identified Loophole | Effect on Pricing | Industry Position |
|---|---|---|
| Exclusion of Specialty Medications | Restricts price reductions on high-revenue drugs | Supports selective compliance |
| Voluntary Rebate Programs | Creates unpredictable consumer savings | Favors negotiation over regulation |
| Extended Appeals Process | Delays enforcement and price adjustments | Advocates for longer review periods |
Calls from Experts for Robust Policy Reforms to Achieve Substantial Price Cuts
Healthcare analysts and policy advocates caution that without enforceable regulations, current drug pricing proposals are unlikely to yield significant savings for patients. They emphasize that the absence of mandatory price ceilings and the dependence on voluntary negotiations severely limit governmental leverage over pharmaceutical companies. Experts argue that effective reform must simultaneously address transparency, competition, and pricing mechanisms.
Recommended policy improvements include:
- Implementing binding price caps on critical medications
- Expanding MedicareŌĆÖs negotiation authority beyond existing limits
- Introducing penalties for unjustified price increases to deter exploitative practices
- Facilitating generic drug market entry through expedited FDA approvals
| Proposed Reform | Projected Impact | Current Status |
|---|---|---|
| Price Caps on Insulin | Potential to reduce costs by up to 40% | Under Review |
| Broaden Medicare Negotiation Powers | Could save $100 billion over 10 years | Not Yet Implemented |
| Penalties for Price Gouging | Discourages excessive price hikes | Proposed |
Conclusion: Navigating the Complexities of Drug Pricing Reform
As the national conversation around prescription drug affordability intensifies, the limitations of TrumpŌĆÖs pricing plan underscore the challenges inherent in reforming the pharmaceutical industry. While the initiative signaled a commitment to reducing medication costs, its dependence on regulatory threats without enforceable measures has drawn criticism for potentially falling short of delivering meaningful relief. The ongoing policy debates will be pivotal in shaping whether future efforts can effectively alleviate the financial burden on American consumers facing high drug prices.